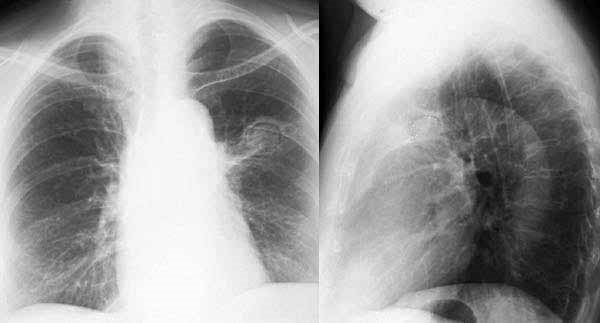
1) A 35 years male, who was admitted in your hospital with the following X-ray, he complained regarding recurrent massive hemoptysis. He was diagnosed as a case of post-PT fibrosis with aspergilloma? How will you counsel him?
|
Greetings & self-introduction |
0.5 |
|
Discussion about disease |
1.0 |
|
Discussion about , control of haemoptysis |
2.0 |
|
Discussion about other medical/ conservative management |
2.0 |
|
What may be the possible complications , if not treated properly . |
2.0 |
|
Discussion about surgical management |
1.5 |
|
Feedback |
1.0 |
2) A 35 years female is suffering from low back pain for two months . She is also suffering of left lower limb for one week . She comes to you with following X-ray .

- Describe the X-ray . What is your diagnosis ?
- Destruction and decrease height of adjacent vertebral bodies . Destruction is more prominent in anterior part of vertebral bodies .
- Disc space between adjacent vertebrae are reduced .
- What are the possible differential diagnosis ?
- Tubercular spondylitis (Pott’s disease).
- Pyogenic osteomyelitis.
- Metastasis.
- What are the relevant investigations , should be advised by you ?
- CT guided FNAC from vertebral lesion .
- Mantoux test and X-ray chest P/A view.
- MRI of vertebral column .
- Write the possible complications , if the patient is not treated properly .
- Paravertebral abscess .
- Cord compression followed by paraplegia.
- Write your management plan .
- Anti tubercular drug.
- If there are features of cord compression , surgical intervention is required .
3. How will you counsel a 28 years old male patient who will receive CAT-Il anti-TB drugs for smear positive PTB?
Checklist:
|
Greetings & self-introduction |
0.5 |
|
Discussion about disease |
1.0 |
|
Discussion about drug |
1.0 |
|
Indication: why prescribed |
1.0 |
|
Side effects |
1.0 |
|
Assurance about side effects |
1.0 |
|
Duration of treatment and time of follow up |
1.0 |
|
Where will you get drugs/DOT |
1.0 |
|
What will happen if there is incomplete treatment |
1.0 |
|
Aware about use of mask |
0.5 |
|
Feedback |
1.0 |
4. Show the procedure of correct use of metered dose inhaler (MDI) with and without spacer and spacer with mask to an asthma patient?
- Correct use of MDI…………………………………………………………….6
- Shake and position of device in between thumb and index finger
- Exhale
- Place the mouth piece in between lips
- Coordination in between deep inspiration and pressure over canester
- Hold the breath for 10 sec, wash mouth after using device.
- Repeat the procedure after 2 minutes interval
- Correct use of spacer ………………………………………………………..3
- Shake the device
- Fixed with spacer
- 1 puff and 5 times breathing in spacer.
- It is better to hold the breath 4 to 10 sec during inspiration.
- Repeat it for next puff .
- Use of spacer with mask …………………………………………………..1
5. A 30 year old man known case of right middle lobe bronchiectasis admitted in your unit with massive haemoptysis. Previously he was admitted in local hospital three times for recurrent infective exacerbation . How will you manage him?
Checklist:
|
Initial management with A, B and C (Air way , Breathing and Circulation : I/V channel open , Blood grouping ) |
2.0 |
|
Advice regarding posture of the patient |
1.0 |
|
Discussion about medical management : 1) Control of infection 2) Postural drainage (contraindicated) |
2.0 |
|
Discussion about surgical management |
2.0 |
|
If surgical intervention not possible (eg. Bronchial artery embolization). |
1.0 |
|
Vaccination |
2.0 |
6. Look at the picture- This man came in OPD with the complain of cough , left sided chest pain and recurrent haemoptysis for two months .

- What are the findings of the above pictorial?................................................................2
- Partial ptosis
- Miosis
- Enopthalmus
- Is there any name of this clinical presentation? What are the other components of this presentation ?................................................................................................................2
Horner’s Syndrome . Anhydrosis .
- What may be the underlying cause?................................................................................3
Left sided bronchial carcinoma .
- What is the possible site of lesion?.................................................................................2
Involvement of left sided sympathetic chain .
- Mention two important investigations for this patient. ..................................................1
CT scan of chest , CT guided FNAC and Fiber optic bronchoscope (FOB)
7. This is an X-ray chest P-A view of 35 years old man who presented with fever, cough and occasional scanty haemoptysis for one month. There was a cavitary lesion in right upper zone .

- What is your diagnosis ? Describe the X-ray . .........................................................................3
PTB (Bilateral) . Bilateral patchy opacity involving upper zones with a cavitary lesion in right side.
- What are the other causes of cavitary lung lesion ?...............................................................2
Infective : MTB, NTM , bacterial, fungal . Vasculitis : WG, RA. Neoplastic : bronchial carcinoma . Non –hodgkins lymphoma .
- What are the radiological signs of active pulmonary tuberculosis ?......................................2
Increasing patchy opacity /soft shadow in serial X-ray , cavitary lesion , pleural effusion etc.
- How will you differentiate malignant cavity from tubercular cavity ?....................................3
Malignant cavity : Thick wall , acentric cavity , minimal fluid , surrounding inflammation absent , irregular inner and outer margin.
8. Read CT scan of chest.

- What are the findings?..................................................................5X2= 10
- A cavitary lesion with crescentic air shadow in right lung.
- What is the likely diagnosis?
- Aspergilloma.
- Mention the presenting feature.
- Asymptomatic
- Haemoptysis
- What are the treatment options?
- If asymptomatic, no treatment is required.
- If massive/recurrent haemoptysis, surgery.
- Name two treatment options if surgery is not possible.
- Local instillation of Amphotericin B.
- Bronchial artery embolization.
9. Look at the spirometric reading given below:
|
|
Predicted |
Test |
% Predicted |
Post-bronchodilator |
% Test |
|
FVC |
3.91 |
3.59 |
92.0 |
4.61 |
+28.4 |
|
FEV1 |
3.14 |
1.42 |
45.2 |
2.01 |
+41.7 |
|
FEV1/FVC |
77.3 |
39.5 |
51.1 |
43.6 |
|
- What type of disease it is ?.........................................................................2X5 = 10
- Obstructive airway disease .
- Is the reversibility test positive ? If it is positive, what are the criterias ?
- Positive , FEV1 increase > 200 ml and FEV1> 12 %
- What is your diagnosis ?
COPD with reversibility component (ACOS)
- Draw an expiratory loop of flow volume curve of obstructive air way disease and a restrictive air way disease .
- What is the basic component of management of your possible diagnosis ?
Inhaled corticosteroid (ICS) and bronchodilator.
10. Look at the picture.
- What is your finding ?.................................................................................................. 5X2 =10
- Dilated veins in upper part of chest .
- What is the most likely diagnosis?
- SVCO.
- What may be the complains of the patient?
Swelling of face and neck , headache (morning , aggravate in bending forward ), dysphagia, stridor , shortness of breath etc.
- What are the most likely causes of this condition?
Bronchial carcinoma , lymphoma , metastatic mediastina lymphadenopathy, retro-sternal goiter
- How will you investigate the patient ?
- X-ray chest , CT scan of chest , Ct guided FNAC , FOB , EBUS-TBNA.
11 .A patient with very sever COPD came with following ECG .
- Mention three important findings...................................................................5X2 = 10
- Tall p wave in lead II
- Tall R wave in lead V1
- Right axis deviation
- Asymmetrical T wave inversion (strain pattern) in II , III , aVF and V1- V4
- What is the most possible cause?
- COPD with right ventricular hypertrophy due to pulmonary hypertension.
- Patient may have right parasternal heave , what are the other impotant findings may present in precordium ?
Palpable P2 , loud P2 , Pansystolicmurmurin tricuspid area , ejection systolic murmur in pulmonary area .
- How you will manage the case ?
- Optimum management of COPD, LTOT, Diuretic etc .
12. Look at the transverse section of HRCT of Chest .
- What are the findings of the above HRCT scan? .......................................................... 5X2 = 10
Multiplering shadows inboth lung fields .
- What is the likely diagnosis?
Bilateral bronchiectasis .
- Mention two important signs of this patient
Bilateral coarse crepitation , altered with cough and clubbing .
- Mention four important presentation of this patient.
Asymptomatic , cough with profuse sputum , haemoptysis ,corpulmonale.
- Mention treatment options of this patient
Postural drainage, control of infection .
13. A 62 years old man presented to a pulmonologist with cough for 3 months, shortness of breath for 15 days and having an X-ray chest P-A view , showing left sided opaque hemithorax .
- Describe the bronchoscopic view of this picture ?..................................................5X2 =10
Left sided endobronchial mass lesion completely occluding the lumen of left principal bronchus.
- Is the carina normal ?
Normal and sharp .
- If it is a Non small cell carcinoma, is surgical treatment possible ?
Not possible (as the mass lesion is within 2 cm of carina ) .
- How will you give palliative management for shortness of breath ?
Thermo plasty / Argon plasma coagulation (APC) followed by stenting.
14. A 60 years old man presented to pulmonologist with persistent dry cough for six months and exortional shortness of breath for three months. The physician found following characteristics in HRCT of chest .
- If there is no etiological factor , what type of ILD is it ?......................................5X2=10
IPF
- Mention the characteristic features in HRCT of chest .
Reticular shadow , subpleural cyst , honey combing , peripheral distribution , less Ground glass opacity(GOO), traction bronchiectasis .
- What physical findings you may get in this patient ?
Cyanosis , clubbing , bilateral fine end inspiratory creps not altered with cough .
- Mention the findings you may get in spirometry, DLCO and six minute walk test .
FEV1/FVC normal or increased , FVC – decreased , DLCO –decreased , SMWT- desaturation
15. A 25 years female come with the complain of arthralgia , fever and dusky colour painful nodular swelling over the shin for last two weeks . She also developed red eye in last two days . HRCT of chest of the patient was as follows .
- Describe the HRCT findings . What is your diagnosis ?
- Bilateral symmetrical hialar lymphadenopathy with nodular shadow distributed along the bronchovascular bundle.
- Sarcoidosis .
- What are the other investigations ,you want to advise to this patient ?
- Mantoux test
- Serum Ca level
- Serum ACE level
- Investigations according to organ involvement.
- What may be the neurological manifestations of this patient ?
Peripheral neuropathy , mononeuritis , cerebellar ataxia , hydrocephalous .
- What may be the findings if the patient perform spiromertry ?
Usually restrictive pattern if parenchyma is involved
Normal if parenchyma is normal
In some cases obstructive may be due to hyper reactive air way .
- Give your management plan .
NSAID and systemic steroid .
16 . A 71 years , male Wt :88kg , Ht :175cm and BMI 28.7 kg/m2, comes to you with the following spirometry tracing .
|
|
Normal |
Observed |
%predicted |
Post-dilator |
|
Spirometry FVC(l) FEV1(l) FEV1/ FVC(%) FEF25-75(L/s) MVV(L/min) Volumes TLC(L) RV/TLC(%) DLCO(mL/min per mm Hg)
|
4.29 3.29 77 2.8 125
6.61 35 25 |
1.94* 1.03* 53* 0.4* 51*
9.37* 75* 10* |
45 31
15 41
142 214 40 |
2.76 1.25
0.5 |
This patient had a smoking history of 74 pack-years and was still smoking. He complained of progressive breathlessness and wheezing on mild exertion. He had a family history of pulmonary disease.
- How would you interpret test?
Severe obstructive air way disease
- Is the test is reversible ?
Reversible
- Can you make a statement as to the patient’s underlying lung disease?
COPD with emphysema predominant with significant reversible component (ACOS)
- Does the reduced DLCO suggest anything?
Presence of significant emphysema .
- What is your management plan ?
Inhaled bronchodilator with inhaled corticosteroid .
17. A 65 years an edentulous patient comes with high grade fever , FOB done under local anesthesia , showing following view .
- Describe the radiological images of X-ray chest P/A view .
Collapse of middle lobe , obscuring the right heart border (Silhoutte sign).
- The patient , initially was diagnosed as lung abscess . What was the possible mechanism of developing lung abscess ?
Distal to the obstruction there was recurrent /persistent infection lead to abscess formation .
- What are the other conditions , lung abscess should be assessed by FOB ?
Atypical location of abscess , thick wall abscess cavity, absence of evidence of infection , suspected case of foreign body inhalation .
- If it is a Non small cell carcinoma and N1 and M0 , what should be your management plan ?
Surgical intervention (lobectomy/pneumonectomy)
- Describe the Role of PET-CT here .
Detection of location of neoplasm , lymphnode involvement and distal metastasis .
18. This is an X-ray of 35 years old man who presented with fever, cough and scanty haemoptysis for one month. He took anti TB drugs two times but could not show any document.
- What are the findings of X-ray above? Marks- 02
- Cavitary lesion in right upper zone
- Patchy opacities on both apices
- What may be the possible diagnosis of this patient? Marks- 02
- PTB (relapsed)
- How will you manage him before getting microbiological report? Marks- 02
- Antibiotic
- Control of haemoptysis
- Antipyretic
- General management
- Name two important investigation for this patient Marks- 1+1
- Sputum for AFB
- Sputum for geneXpert
- What is the next step if sputum AFB is 2+ and 3+ but gene Xpert is negative? Marks- 02
- Sputum AFB culture for both typical and atypical mycobacteria.
19. Look at the picture :
a) Write the name of the device . Write the characteristic features of it .
Intrathoracic Tube . It has two ends . One end is introduced within thoracic cavity another end is connected to water seal drainage . There are multiple lateral opening near the first end . The tube is marked in cm . There is a radio opaque line in the tube .
b) Write the utilities of the device .
Evacuation of unwanted air (pneumothorax) , pleural fluid (pleural effusion) , pus (empyema thoracis) , blood (haemothorax in trauma , post surgical).
c) Describe the insertion site .
In 4th and 5th intercostal space within triangle of safety (between anterior and posterior axillary fold)
d) How will you follow up the cases ?
Daily amount of fluid is evacuated, movement of fluid column in tube (for presence of fistula), clinical examination of chest , chest X-ray.
e)Write complications of the procedure .
Haemorrhage (trauma to intercostal vessel), vasovagal attack , lung injury , trauma to underlying structure according to insertion site (diaphragm , spleen , liver etc) , infection (eg. Empyema).
20. Interpret the ECG
- What is your diagnosis ? Describe the characteristics features of this ECG .
Atrial fibrillation . Absence of P wave and QRS complexes are in irregular interval .
- What clinical findings will you get in this case ?
Pulse : irregularly irregular , pulsus deficit present ,features associated with underlying cause .
- What are the preferable investigations in this case ?
X-ray chest P/A view , Echocardiography.
- Write some respiratory causes of this ECG findings .
Pneumonia , COPD etc
- What are the other causes of this ECG findings ?
Mitral valvular disease (MS,MR) , Hyper thyroidism , cardiomyopathy , Lone atrial fibrillation .
21) Look at the transverse section of CT scan of chest in mediastinal view with contrast enhancement .
- Describe the picture .
Anterior mediastinal mass encasing the great vessels and compressing large air ways.
- What is your differential diagnosis .
- Lymphoma 2) Thymoma 3) Teratoma
- What are the clinical findings you may get in this patient ?
- Chest pain 2) Shortness of breath 3) Dysphagia 4) SVCO
- Write the methods of collection of sample from the lesion for tissue diagnosis .
1) CT guided FNAC 2) EBUS and TBNA 3) Mediastinoscopy
e) What medical emergency may arise in this patient ?
Compression of airway leading to shortness of breath , stridor followed by asphyxia .


Comments